Why Medical Imaging Professionals Are Essential to Modern Healthcare
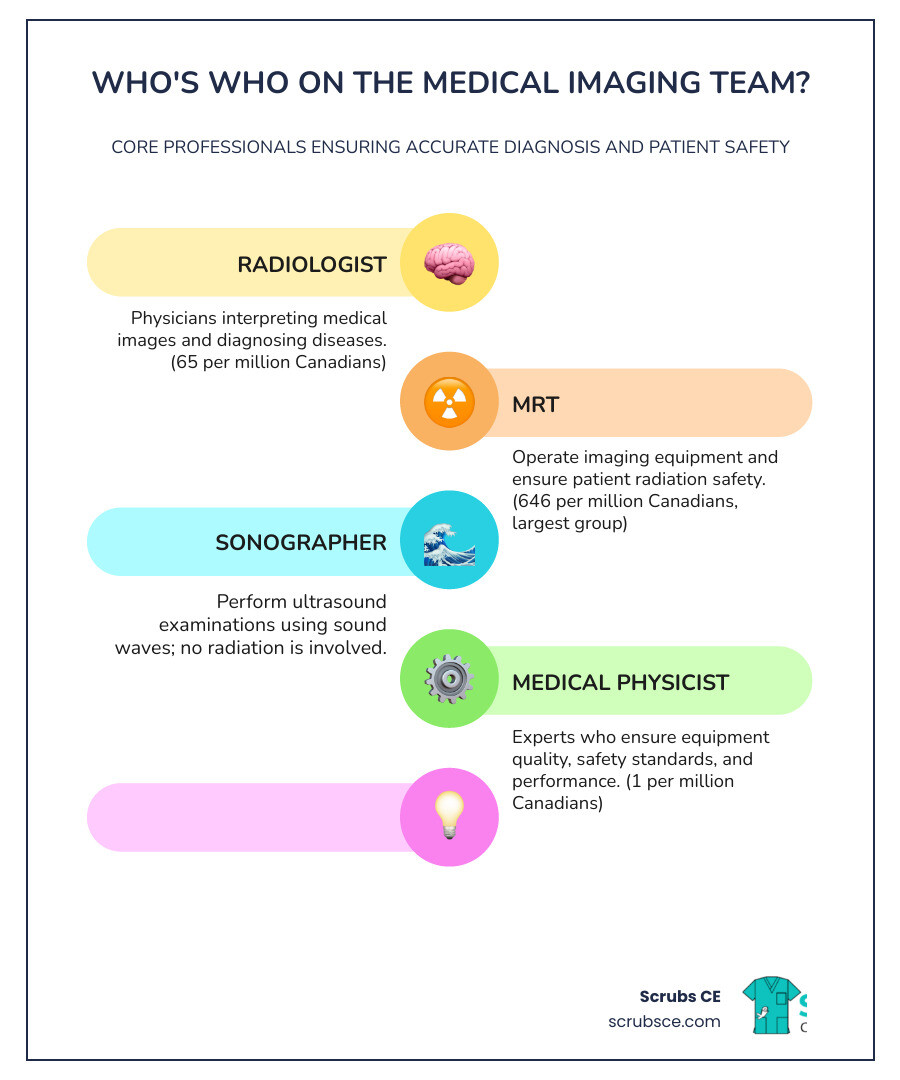
Medical imaging professionals are the specialized healthcare workers who operate diagnostic equipment, interpret medical images, and ensure patient safety during procedures like X-rays, CT scans, MRIs, and ultrasounds. These professionals form a collaborative team that includes:
- Radiologists – Physicians who interpret medical images and diagnose diseases
- Medical Radiation Technologists (MRTs) – The largest group, operating imaging equipment and ensuring radiation safety
- Sonographers – Specialists who perform ultrasound examinations using sound waves
- Diagnostic Medical Physicists – Experts who ensure equipment quality and safety standards
Medical imaging has become one of the fastest-growing medical specialties today. Most Canadians have undergone a medical imaging procedure or know someone who has, yet few understand the diverse team of professionals working behind the scenes to make accurate diagnosis possible.
The field is experiencing unprecedented challenges. Since 2004, CT exam volumes have increased by 131% and MRI exams by 188%, but the workforce has only grown by 64%. This gap has led to longer wait times, increased burnout among professionals, and equipment sitting idle due to staffing shortages. In Canada, the median wait time for a CT scan jumped from 26 days in 2012 to 46 days in 2023 – a 77% increase.
I’m Zita Ewert, and through my work leading SCRUBS Continuing Education, I’ve spent years supporting medical imaging professionals with the training and CE credits they need to maintain certification and advance their careers. Understanding the roles, challenges, and career pathways in this field has never been more important for both aspiring professionals and those already working in the industry.
Who’s Who on the Medical Imaging Team?
When you undergo a medical imaging procedure, you’re not just interacting with a single individual; you’re benefiting from the expertise of a highly specialized and collaborative team. This team works together seamlessly to ensure accurate diagnoses, effective treatments, and, most importantly, your safety and well-being. Each member plays a crucial role in the patient care pathway, contributing their unique skills to the diagnostic process. While their work environments might vary, from busy hospital departments to specialized clinics, their shared goal is to provide the best possible care.
Radiologists and Nuclear Medicine Specialists
At the helm of the medical imaging team are the Radiologists and Nuclear Medicine Specialists. These are physicians who have undergone extensive medical training, including medical school and specialized residencies, to become experts in interpreting medical images.
A Radiologist is a medical doctor dedicated to diagnosing and treating diseases and injuries using sophisticated medical imaging techniques. As highlighted by the American College of Radiology, these techniques include X-rays, Computed Tomography (CT), Magnetic Resonance Imaging (MRI), Positron Emission Tomography (PET), fusion imaging, and ultrasound. Their role extends far beyond simply “reading” images; they act as expert consultants to referring physicians, helping to select the most appropriate examinations, interpreting the findings, correlating them with other clinical tests, and even recommending further steps in your care. Some Radiologists also perform image-guided interventions or deliver radiation therapy. Their training is rigorous, typically involving at least four years of postgraduate medical education after medical school, with many pursuing an additional one to two years of fellowship training in a subspecialty. This depth of knowledge ensures that your medical images are interpreted with the highest level of expertise. You can learn more about their vital role at What Is a Radiologist?.
Within Radiology, there are numerous subspecialties, allowing for even deeper expertise. These include:
- Interventional Radiology: Physicians who perform minimally invasive, image-guided procedures to diagnose and treat diseases in nearly every organ system.
- Pediatric Radiology: Specializing in the imaging diagnosis of diseases in infants, children, and adolescents.
- Neuroradiology: Focusing on the diagnosis of disorders of the brain, spine, head, and neck using imaging techniques.
- Breast Imaging: Specializing in mammography, breast ultrasound, and breast MRI for the diagnosis and staging of breast cancer.
- Cardiovascular Radiology: Diagnosing heart and circulatory system diseases.
- Musculoskeletal Radiology: Specializing in disorders of bones, joints, and soft tissues.
Nuclear Medicine Specialists are also physicians, but their expertise lies in using small amounts of radioactive materials, known as radiopharmaceuticals, to diagnose and treat a wide range of diseases. These specialists understand radiation biology, radiopharmacy, and nuclear physics. They use modalities such as Single Photon Emission Computed Tomography (SPECT), PET, and hybrid imaging technologies like SPECT-CT and PET-CT to visualize organ function and molecular activity, often detecting diseases at their earliest stages.
Medical Radiation Technologists (MRTs)
The largest professional group within the advanced imaging workforce are the Medical Radiation Technologists (MRTs). In Canada, there were 25,752 full-time equivalent (FTE) MRTs practicing in 2022–2023, making them the backbone of many imaging departments. These dedicated professionals are often your first point of contact in an imaging department, and their role is incredibly hands-on and patient-focused.
MRTs are responsible for operating complex imaging equipment, accurately positioning patients, and ensuring the quality of the images produced. But their job isn’t just technical; it’s also about communication and care. They explain procedures to patients, answer questions, and ensure comfort and safety throughout the examination. A critical aspect of their work, especially in modalities using ionizing radiation, is adhering to the ALARA principle – “As Low As Reasonably Achievable” – to minimize radiation exposure for both patients and themselves. This involves using radiation protective devices and precise collimation techniques.
MRTs typically specialize in one of four disciplines:
- Radiological Technology: Performing general X-rays, fluoroscopy, and CT scans.
- Magnetic Resonance (MR) Imaging: Operating MRI scanners, which use powerful magnets and radio waves to create detailed images of organs and soft tissues.
- Nuclear Medicine Technology: Administering radiopharmaceuticals and operating SPECT and PET scanners to capture images of physiological processes.
- Radiation Therapy: Planning and delivering radiation treatments to patients with cancer, working closely with radiation oncologists and medical physicists.
The Canadian Association of Medical Radiation Technologists (CAMRT) provides invaluable resources and practice guidelines for MRTs, ensuring high standards of care across the country. You can explore these guidelines at View More Practice Guidelines.
Sonographers (Ultrasound Technologists)
Sonographers, also known as ultrasound technologists or technicians, are the experts in operating equipment that uses high-frequency sound waves to capture images of a patient’s internal organs and tissues. What makes their role unique is that ultrasound imaging does not use ionizing radiation, making it a safe choice for many patients, including pregnant individuals.
These professionals work directly with patients in various settings, including hospitals, outpatient clinics, and physician offices. Their responsibilities include preparing the ultrasound equipment, explaining the procedure to the patient, positioning them correctly, and skillfully manipulating the transducer to acquire the necessary diagnostic images. Sonographers require a keen eye and strong anatomical knowledge to produce clear, interpretable images that radiologists can then diagnose from.
Sonographers can specialize in many areas, such as:
- Abdominal Ultrasound: Imaging organs like the liver, gallbladder, kidneys, and pancreas.
- Echocardiography: Specializing in heart imaging.
- Vascular Ultrasound: Examining blood vessels for blockages or other issues.
- Obstetrics and Gynecology: Performing ultrasounds during pregnancy and for gynecological health.
- Musculoskeletal Ultrasound: Imaging muscles, tendons, and ligaments.
For more in-depth information on the profession of sonography, we recommend visiting the Society of Diagnostic Medical Sonography.
Diagnostic Medical Physicists
While often working behind the scenes, Diagnostic Medical Physicists are indispensable members of the medical imaging team. They are highly specialized scientists with advanced degrees, typically a doctorate or master’s, and extensive clinical physics training.
Their primary role is to ensure the safety and quality of medical imaging equipment and procedures. This includes:
- Equipment Quality Control: Regularly testing and calibrating imaging devices like CT scanners, MRI machines, and X-ray units to ensure they function optimally and produce high-quality images.
- Safety Assurance: Implementing and overseeing radiation safety programs, ensuring that equipment adheres to strict safety standards, and minimizing radiation exposure for patients and staff.
- Performance Audits: Conducting comprehensive audits of imaging systems and processes to identify areas for improvement and maintain accreditation standards.
- Technical Expertise: Providing expert advice on the selection, installation, and shielding of new imaging equipment, as well as collaborating on the development of new imaging techniques.
Diagnostic Medical Physicists are certified by boards like the American Board of Radiology or the American Board of Medical Physics, signifying their high level of training and expertise. In Canada, there were 45 imaging medical physicists practicing in 6 provinces in 2022–2023, underlining their specialized and critical contribution to the field.
Pathways to a Career in Medical Imaging
The field of medical imaging is dynamic and rewarding, offering diverse career paths for individuals passionate about healthcare and technology. Regardless of the specific role, certain fundamental skills are highly valued: excellent communication and listening abilities, a strong sense of responsibility and organization, a natural technical aptitude, and the capacity for teamwork. Working in this field often involves physical tasks and handling medical instruments, so a comfort with such activities is also beneficial.
Educational and Training Requirements for Medical imaging professionals
The educational journey for medical imaging professionals varies significantly depending on the chosen specialty, reflecting the depth and breadth of knowledge required for each role.
-
Radiologist Path: This is the longest and most intensive pathway. It begins with a bachelor’s degree, followed by four years of medical school (MD or DO). After obtaining their medical degree, aspiring Radiologists complete a one-year internship and then a four to five-year residency program in Diagnostic Radiology. Many then pursue an additional one to two-year fellowship in a subspecialty, such as Neuroradiology or Interventional Radiology, to gain even more specialized expertise.
-
Medical Radiation Technologist (MRT) Path: For MRTs, the educational requirements typically involve a college diploma or a bachelor’s degree in medical radiation sciences. These programs, often two to four years in length, provide comprehensive training in anatomy, physiology, radiation physics, patient care, and the operation of various imaging modalities. In Quebec, for instance, diagnostic imaging training programs are offered in several regions, preparing students for roles in Diagnostic Radiology, nuclear medicine, and radiation oncology. You can explore these programs further through resources like Diagnostic imaging training programs.
-
Sonographer Path: Sonographers typically complete at least a two-year formal education program, often leading to an associate’s or bachelor’s degree in diagnostic medical sonography. For those with prior healthcare experience, one-year certificate programs are also available. These programs focus on ultrasound physics, cross-sectional anatomy, and clinical practice, providing the hands-on skills needed to perform detailed ultrasound examinations.
-
Diagnostic Medical Physicist Path: This path requires a strong foundation in physics. Professionals typically earn a master’s or doctoral degree (Ph.D.) in medical physics or a related field. This is followed by one to two years of clinical physics training, often in a residency program, to gain practical experience in the clinical environment, ensuring the safe and effective use of radiation in medicine.
Certification and Licensing
Beyond formal education, medical imaging professionals must obtain specific certifications and licenses to practice. These credentials ensure that individuals meet national and provincial standards of competence and professionalism.
-
National Certification Exams: Most medical imaging professionals must pass national certification examinations. For example, MRTs in Canada are certified by organizations like the Canadian Association of Medical Radiation Technologists (CAMRT), while Radiologists in North America are typically board-certified by the American Board of Radiology or the American Osteopathic Board of Radiology. Sonographers are often certified by the American Registry for Diagnostic Medical Sonography (ARDMS). These certifications demonstrate a high level of training and expertise in their respective fields.
-
Provincial Regulatory Bodies: In Canada, each province and territory has regulatory bodies that oversee the practice of medical imaging professionals. These bodies grant licenses to practice, ensuring that professionals adhere to provincial standards and codes of ethics. For instance, Quebec has the Ordre des technologues en imagerie médicale, en radio-oncologie et en électrophysiologie médicale du Québec, which regulates technologists in the province. You can find more information about their role at Quebec’s regulatory body for technologists.
-
Importance of Credentials: Holding valid certification and licensing is crucial for several reasons. It assures patients and employers of a professional’s competence, it’s often a legal requirement for employment, and it provides a framework for professional accountability.
-
Continuing Education Requirements: The field of medical imaging is constantly evolving with new technologies and techniques. Therefore, medical imaging professionals are typically required to complete ongoing continuing education (CE) credits to maintain their certification and licensing. This ensures they stay current with the latest advancements and best practices, constantly refining their skills and knowledge. This commitment to lifelong learning is something we deeply understand and support at Scrubs CE.
The State of the Workforce: A Canadian Perspective
The landscape of medical imaging in Canada is characterized by a significant and growing imbalance between demand for services and the availability of qualified medical imaging professionals. This disparity has profound implications for patient care and the sustainability of the healthcare system.
Since 2004, the volume of medical imaging exams has surged dramatically. CT exam volumes in Canada have increased by an astounding 130.7%, and MRI exam volumes have seen an even more staggering rise of 188.2%. This rising demand is driven by several factors, including an aging population, increased prevalence of chronic diseases, and advancements in medical science that make imaging a crucial diagnostic tool. However, the growth in the workforce has simply not kept pace. Over the same period, the overall number of MRT positions in Canada increased by a comparatively modest 64.4%. This slower workforce growth relative to the escalating demand creates immense pressure on the existing medical imaging professionals and the entire healthcare system.
Current Staffing Levels and Trends
The latest data from 2022–2023 paints a clear picture of the current staffing landscape for medical imaging professionals in Canada.
- Medical Radiation Technologists (MRTs): Comprised the largest group, with 25,752 FTE MRTs practicing across all 13 provinces and territories. This translates to approximately 646 FTE MRTs per million people in Canada.
- Radiologists: There were 2,602 Radiologists practicing in all 13 provinces and 1 territory, which is about 65 Radiologists per million people.
- Nuclear Medicine Specialists: A smaller, highly specialized group, with 284 specialists practicing in 9 provinces, or approximately 7 per million people.
- Imaging Medical Physicists: The most specialized group, with only 45 physicists practicing in 6 provinces, equating to about 1 per million people.
These numbers, while informative, also highlight significant geographic variations. The distribution of medical imaging professionals is not uniform across the country, with some regions experiencing greater shortages than others, particularly in rural and remote areas. The Canadian Medical Imaging Inventory (CMII) provides comprehensive data on these trends, which is crucial for understanding and addressing these disparities. You can dig deeper into these findings in the Canadian Medical Imaging Inventory 2022–2023 Report.
The Impact of Staffing Shortages on Patient Care
The gap between escalating demand and insufficient workforce growth has tangible and often severe consequences for patient care.
- Increased Wait Times: One of the most direct impacts is the significant increase in patient wait times for critical imaging procedures. Between 2012 and 2023, the median wait time for a CT scan in Canada increased by 77%, from 26 to 46 days. For MRI scans, the situation is even more pronounced, with wait times increasing by 53%, from 59 to 90 days over the same period. These delays mean patients wait longer for diagnoses, which can postpone treatment and potentially worsen health outcomes.
- Service Disruptions: Staffing shortages lead to disruptions in service delivery. We hear reports of CT scanners sitting idle, even newly purchased ones, because there aren’t enough qualified medical imaging professionals to operate them. This is a heartbreaking reality where valuable equipment, meant to save lives, cannot be fully used.
- Delays in Diagnosis and Treatment: Prolonged wait times and service disruptions inevitably lead to delays in diagnosis and, consequently, delays in starting necessary treatments. For conditions where early diagnosis is critical, such as cancer, these delays can have serious, even life-threatening, implications. Patients are left in limbo, experiencing anxiety and uncertainty while waiting for essential imaging results.
Key Challenges and Future Directions for Medical imaging professionals
The current state of medical imaging in Canada presents a clear workforce crisis, demanding immediate and sustained attention to ensure the health and sustainability of our healthcare system. This isn’t just about numbers; it’s about the well-being of the dedicated medical imaging professionals and the patients they serve.
Burnout, Workload, and Professional Well-being
The statistics are stark: since 2018, medical imaging professionals have reported a staggering 42% increased workload. Imagine the pressure of seeing patient volumes rise relentlessly while your team remains understaffed. This translates directly into increased stress, emotional exhaustion, and a significant decrease in feelings of trust, respect, and safety in the workplace, down by up to 25%.
A national mental health survey of Medical Radiation Technologists (MRTs) conducted between 2018 and 2023 revealed alarming trends:
- Emotional exhaustion increased by 94%.
- Depersonalization, a feeling of detachment from one’s job and patients, soared by 106%.
- Feelings of reduced personal accomplishment grew by 21%.
- There was a twofold increase in the number of participants reporting a serious mental health issue.
These figures underscore a profession pushed to its limits. The consequences are evident in skyrocketing vacancy rates for MRT positions, which have increased more than two-fold for CT, three-fold for nuclear medicine, and four-fold for MRI since 2018. This vicious cycle of understaffing leading to burnout, which in turn exacerbates shortages, threatens the very foundation of medical imaging services.
Strategies to Address the Crisis
Addressing this complex crisis requires a multi-faceted approach, combining strategic investments, policy changes, and a renewed focus on the well-being of medical imaging professionals.
- Investing in technology and AI: Embracing advancements like Artificial Intelligence (AI) in image analysis and workflow automation tools can alleviate some of the workload burden on professionals. AI can assist in prioritizing studies, detecting anomalies, and improving efficiency, allowing medical imaging professionals to focus on complex cases and patient interaction.
- Improving recruitment and retention policies: Robust strategies are needed to attract new talent to the field and, crucially, to keep experienced professionals from leaving. This includes competitive compensation, improved work-life balance initiatives, and clear career progression pathways.
- Promoting healthy and respectful workplaces: Creating supportive work environments that prioritize mental health, trust, and respect is paramount. This involves fostering strong leadership, providing adequate resources for stress management, and ensuring that professionals feel valued and heard.
- Reducing low-value imaging (10-25% of exams are unnecessary): A significant portion of medical imaging exams, estimated between 10% and 25% annually, are considered unnecessary or of low value. These exams contribute to increased workload, unnecessary radiation exposure for patients, and inflated healthcare costs. Strategies such as implementing clinical decision support systems and encouraging Radiologists to consult with referring providers can help reduce these unwarranted scans, freeing up valuable resources.
The Role of Technology and Innovation
Technology and innovation are not just about new machines; they are powerful allies in supporting the medical imaging team and improving efficiency.
- AI in image analysis: AI algorithms are becoming increasingly sophisticated, capable of analyzing medical images with remarkable speed and accuracy. They can help identify subtle abnormalities, quantify disease progression, and even predict treatment responses. This augments the capabilities of Radiologists and MRTs, allowing for faster diagnoses and more personalized patient care.
- Workflow automation tools: Beyond image analysis, technology can streamline administrative tasks, scheduling, and reporting, reducing the non-clinical burden on medical imaging professionals. Automated order entry and improved communication platforms can improve operational efficiency.
- Portable scanners for increased access: Innovations like portable low-field MRI scanners offer the potential to expand access to imaging services, particularly in underserved rural and remote areas. These devices can bring essential diagnostic capabilities directly to patients, reducing travel burdens and wait times.
- Clinical decision support systems: These systems provide referring physicians with evidence-based guidance on the most appropriate imaging studies for specific clinical conditions. By ensuring that the right test is ordered at the right time, they help reduce unnecessary exams and improve the overall efficiency of the imaging pathway.
By strategically integrating these technological advancements, we can create a more sustainable and efficient medical imaging system, ultimately benefiting both medical imaging professionals and the patients they serve.
Conclusion
The world of medical imaging is a cornerstone of modern healthcare, providing the critical insights needed for accurate diagnosis and effective treatment. As we’ve explored, medical imaging professionals — from expert Radiologists and Nuclear Medicine Specialists to hands-on Medical Radiation Technologists, meticulous Sonographers, and precision-focused Diagnostic Medical Physicists — form a collaborative, indispensable team. Their dedication ensures that millions of patients receive the care they need, often in moments of uncertainty and vulnerability.
However, this vital sector faces significant challenges, particularly in Canada. The rapid escalation in demand for imaging services, far outstripping workforce growth, has led to concerning increases in patient wait times, service disruptions, and valuable equipment sitting idle. This imbalance has placed immense pressure on our medical imaging professionals, leading to alarming rates of burnout, increased workloads, and a decline in workplace well-being.
Despite these problems, there is a hopeful outlook. The commitment to addressing these issues is strong, with strategies focusing on robust recruitment and retention, fostering healthy work environments, and reducing unnecessary imaging. Crucially, technological innovation, particularly in Artificial Intelligence and workflow automation, holds immense promise for improving efficiency, alleviating workload, and enhancing diagnostic capabilities. These advancements are not meant to replace human expertise but to empower medical imaging professionals to deliver even higher quality, more timely care.
For those considering a career in medical imaging, or for current professionals seeking to maintain and advance their expertise, the importance of ongoing professional development cannot be overstated. Lifelong learning is essential to steer the evolving landscape of this field, accept new technologies, and continue providing exceptional patient care. At Scrubs CE, we are dedicated to supporting this journey by offering convenient, affordable, and high-quality online continuing education courses. We believe that by investing in our medical imaging professionals, we are investing in the future of healthcare.
To further your knowledge and advance your career, explore our specialized courses: Advance your career with Radiology CE courses.



Recent Comments