Why Advanced Breast Imaging Matters More Than Ever
Advanced breast imaging refers to diagnostic techniques that go beyond standard 2D mammography to improve breast cancer detection, particularly for women with dense breast tissue or high cancer risk. These methods include 3D mammography (tomosynthesis), breast MRI, molecular breast imaging (MBI), and emerging technologies like contrast-improved mammography.
Key Advanced Breast Imaging Techniques:
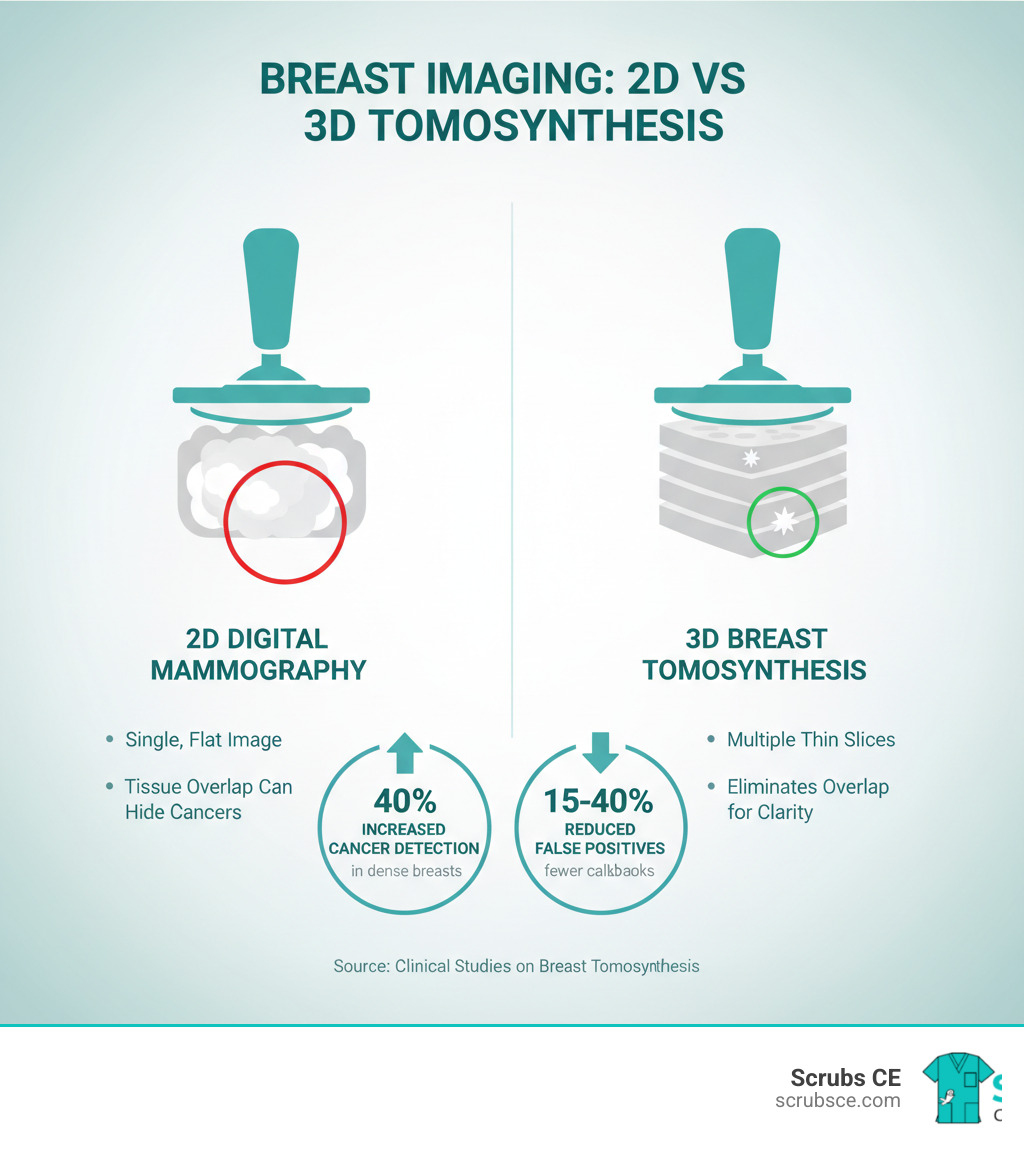
- Digital Breast Tomosynthesis (3D Mammography): Creates layered images to reduce tissue overlap, improving cancer detection and reducing false-positive callbacks by 15-40%.
- Breast MRI: Uses magnetic fields and contrast agents for 90-100% sensitivity, especially valuable for high-risk women.
- Molecular Breast Imaging (MBI): Detects cancer cell activity using radioactive tracers, finding 3x more cancers when combined with mammography in women with dense breasts.
- Contrast-Improved Mammography (CEM): Highlights abnormal blood flow patterns using iodine contrast, offering a faster, less expensive alternative to MRI.
Breast cancer is the most commonly diagnosed cancer among women, with over 287,000 new cases expected annually in the U.S. While traditional 2D mammography has been the standard since the 1970s, its sensitivity drops from 87% in fatty breasts to just 63% in dense breasts—a condition affecting about 50% of women.
This detection gap spurred the development of advanced imaging. These newer methods find more cancers earlier, reduce unnecessary biopsies, and guide more precise treatment. For healthcare professionals, understanding these techniques is essential for providing optimal care and staying current with evolving standards. The shift toward personalized, risk-based screening means that one-size-fits-all mammography is becoming a thing of the past, requiring knowledge of multiple modalities.
Beyond the Standard View: Why Traditional Mammography Isn’t Always Enough
While traditional 2D mammography has saved countless lives, its limitations drive the need for advanced breast imaging.
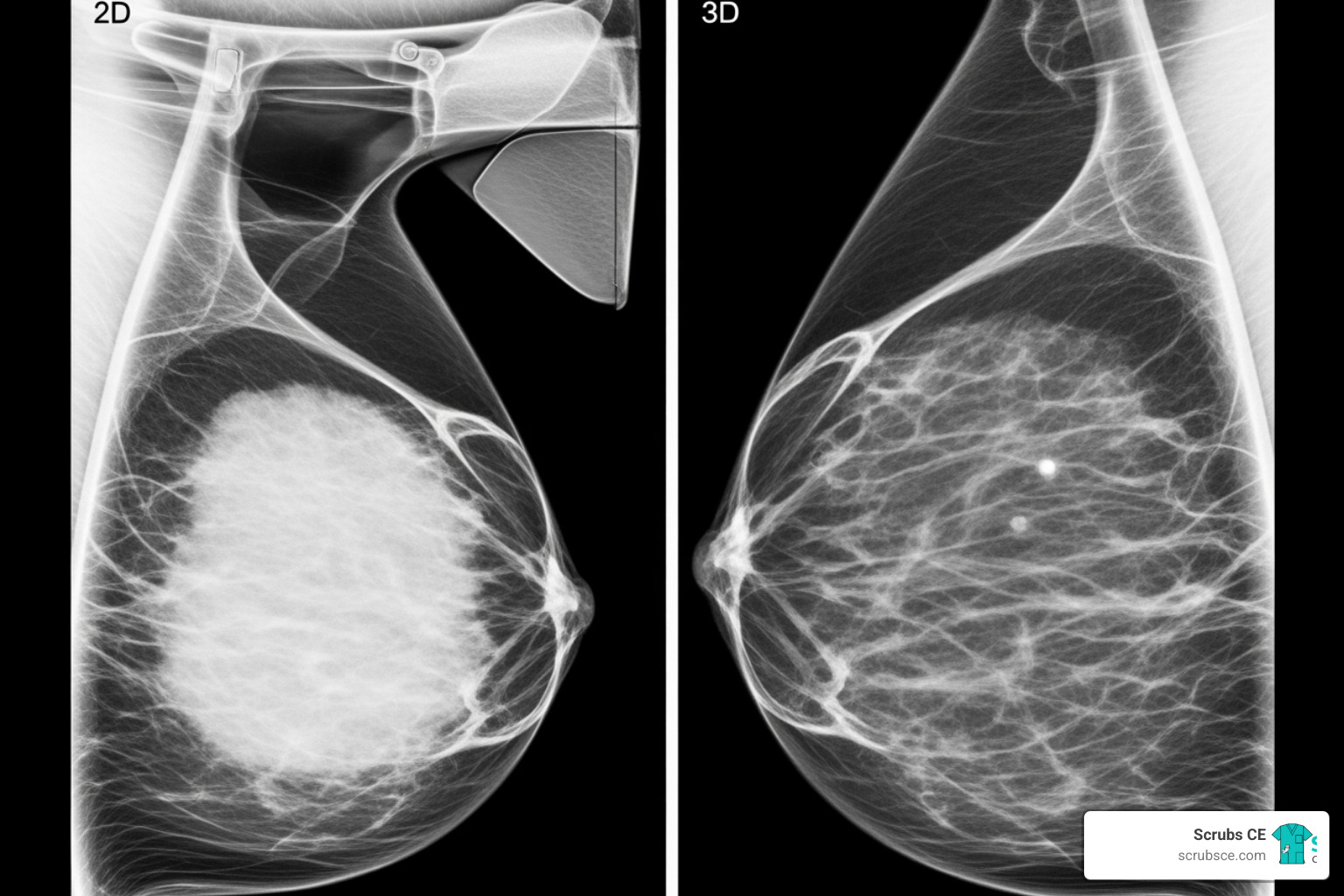
The biggest challenge is dense breast tissue, which affects about half of all women. On a mammogram, both dense tissue and cancer appear white, making it difficult for radiologists to distinguish between them. This is like trying to spot a white golf ball in snow. As a result, mammography’s cancer detection rate drops from 87% in fatty breasts to as low as 50-63% in very dense breasts. You can learn more about how dense breast tissue affects mammography results and its screening implications.
Another issue is tissue overlap. A standard 2D mammogram is a single, flat image where normal breast structures can stack up, creating confusing shadows or hiding cancers. This leads to two frustrating outcomes:
- False-positives: When a mammogram looks suspicious but is ultimately normal. Between 5% and 15% of screened women are called back for more tests, causing anxiety and contributing to the roughly $4 billion spent annually on false-positive follow-ups.
- False-negatives: The more worrisome outcome, where cancer is present but the mammogram appears normal. This is more common in women with dense breasts, allowing a tumor to grow undetected.
These limitations underscore why continuing education is critical. Healthcare professionals must stay current with mammography CE courses to understand when to use advanced techniques. Fortunately, new tools are available to address these challenges.
A Clearer Picture: Key Advanced Breast Imaging Modalities
When traditional mammography is inconclusive, advanced breast imaging provides a clearer picture. These sophisticated techniques improve cancer detection rates, especially in dense breast tissue, and reduce false positives. They enable a move away from a one-size-fits-all approach toward supplemental screening custom to each patient’s risk profile.
Digital Breast Tomosynthesis (3D Mammography): The New Standard in Advanced Breast Imaging
Digital breast tomosynthesis (DBT), or 3D mammography, overcomes the primary limitation of 2D mammography: tissue overlap.
How it works: The X-ray tube moves in an arc over the breast, capturing multiple low-dose images from different angles. A computer reconstructs these into a series of thin image “slices,” each about 1mm thick. Radiologists can scroll through these layers, effectively “seeing through” the breast tissue to spot abnormalities that might otherwise be hidden.
Benefits: DBT improves cancer detection for women of all breast densities and is particularly effective for finding invasive cancers in dense breasts. It also reduces callbacks by 15-40% compared to 2D mammography, meaning less anxiety and fewer unnecessary follow-up appointments for patients.
Radiation dose: The radiation from DBT is slightly higher than a 2D mammogram but remains well within FDA safety limits. The significant improvement in detection is widely considered a favorable trade-off. As DBT becomes more common, healthcare professionals can deepen their expertise through comprehensive Mammography CE Courses.
Breast MRI: High-Sensitivity Detection for Specific Patient Groups
Instead of X-rays, Breast MRI uses magnetic fields and radio waves to create detailed images.
How it works: A contrast agent (gadolinium) is injected into a vein. Cancerous areas, which have increased blood flow, absorb the agent and “light up” on the images. This gives MRI an impressive sensitivity rate of 90-100%, regardless of breast density.
Best uses: This high sensitivity makes MRI the gold standard for screening high-risk women, such as those with a lifetime risk over 20% or BRCA gene mutations. It is also invaluable for:
- Staging known cancer: Determining tumor size and detecting additional cancer sites in the same or opposite breast.
- Guiding treatment: MRI findings influence treatment plans for about 25% of patients, helping to refine surgical approaches or identify candidates for pre-surgical chemotherapy.
Limitations: Breast MRI is expensive, less accessible than mammography, and can have higher false-positive rates that lead to more biopsies. The procedure also requires patients to lie still in a narrow tube for 30-45 minutes. Patients can find more info on breast MRI to understand what to expect.
Molecular Breast Imaging (MBI): A Functional Approach to Detection
MBI focuses on cell function rather than anatomy.
How it works: A small amount of a radioactive tracer is injected, which is absorbed more by active cancer cells. A special gamma camera detects the tracer, creating images that highlight areas of high metabolic activity. Because it focuses on cell activity, breast density does not interfere with its effectiveness.
Benefits: For women with dense breasts, adding MBI to mammography finds three times more cancers than mammography alone. It also has a lower false-positive rate than mammography, reducing unnecessary callbacks and biopsies.
Role: MBI is used as a supplementary test alongside mammography for women with dense breasts. Its radiation dose is comparable to a mammogram and is FDA-approved. As its use grows, it offers a powerful tool for a historically underserved patient group. For more details, see a closer look at molecular breast imaging.
The Future is Now: Emerging and Experimental Techniques
The field of advanced breast imaging is constantly evolving, with researchers exploring new ways to detect cancer earlier and more accurately. These emerging technologies promise to overcome current limitations and improve patient comfort.
Promising Technologies on the Horizon
Several innovative technologies are showing promise in clinical research:
- Contrast-Improved Mammography (CEM): Uses an iodine-based contrast dye to highlight areas of increased blood flow, a common sign of cancer. CEM offers MRI-like information at a lower cost and in less time, making it a promising alternative for diagnostic workups and screening women with dense breasts.
- Ultrasound Elastography: Measures tissue stiffness, as cancerous tumors are typically firmer than benign tissue. This technique can help distinguish between concerning and harmless lesions, potentially reducing unnecessary biopsies.
- Optical Imaging: Uses light instead of radiation to detect abnormalities. By measuring how different tissues absorb and reflect light, this experimental method offers a radiation-free and compression-free approach.
- Electrical Impedance Tomography (EIT): Measures differences in how cancer cells and normal cells conduct electricity. Using small electrical currents, EIT creates a map of conductivity without radiation or compression.
These cutting-edge tools are not yet routine but are moving closer to clinical practice. You can learn more about them from the American Cancer Society’s overview of Newer and Experimental Breast Imaging Tests.
The Role of AI in Advanced Breast Imaging
Artificial Intelligence (AI) is becoming an invaluable partner for radiologists. AI algorithms, trained on millions of images, excel at AI-assisted analysis by flagging suspicious areas that the human eye might miss.
Key applications include:
- Automated tumor segmentation: AI can instantly and precisely outline a tumor’s borders on 3D images like MRI, which is crucial for accurate measurement and monitoring treatment response.
- Improved diagnostic accuracy: By providing a “second opinion,” AI can help reduce false positives and catch subtle cancers, improving overall accuracy without replacing the radiologist’s judgment.
- Reduced workload: AI can triage cases and handle routine analysis, freeing radiologists to focus on complex cases. This is especially helpful in facilities facing staff shortages.
As AI tools evolve, staying current is essential. For those looking to sharpen their interpretation skills, our Breast Imaging Case Review Series offers practical learning from real clinical scenarios. The future lies in combining these innovations for a more comprehensive, patient-centered approach to breast cancer detection.
Clinical Application: Integrating Advanced Imaging into Practice
Knowing about advanced breast imaging technologies is one thing; applying them strategically is another. The goal is to create a personalized screening and treatment roadmap for each patient based on their unique risk factors, breast density, and clinical situation. This approach improves early detection, guides surgical decisions, and helps monitor treatment efficacy.
| Factor | Digital Breast Tomosynthesis (DBT) | Breast MRI | Molecular Breast Imaging (MBI) |
|---|---|---|---|
| Best Use Case | General screening, especially with dense breasts; Diagnostic follow-up | High-risk screening; Staging known cancer; Evaluating treatment response | Supplemental screening for dense breasts (adjunct to mammography) |
| Dense Breast Efficacy | Significantly improved detection, reduced callbacks | Very high sensitivity (90-100%) | Very high sensitivity, density has minimal effect, finds 3x more cancers with mammography |
| Radiation | Slightly higher than 2D mammography, but within safe limits | None (uses magnetic fields and radio waves) | Low-dose radioactive tracer, comparable to mammogram |
| Cost/Access | Becoming more widely available, often covered by insurance | Higher cost, less accessible, can be resource-intensive | Moderate cost, growing availability, often supplementary |
Choosing the Right Test: Factors and Recommendations
Selecting the appropriate imaging test requires considering several factors:
- Patient risk factors: A woman with a lifetime breast cancer risk over 20% (e.g., due to BRCA mutations or strong family history) requires a different strategy than an average-risk woman. For high-risk patients, breast MRI is an essential screening tool.
- Breast density: With breast density notification laws, more patients are aware of their tissue type. For those with dense breasts, supplemental screening with DBT or MBI is crucial for seeing through tissue that can hide cancers.
- Cost and accessibility: Practical realities like insurance coverage and technology availability influence decisions. MRI is expensive and less accessible, while DBT is becoming more common. These factors must be steerd with the patient.
- Radiation exposure: Though doses from DBT and MBI are low and within FDA safety limits, cumulative exposure is a consideration. Clinicians use tools like the ACR Appropriateness Criteria® to make evidence-based choices for specific scenarios, such as ACR Appropriateness Criteria® for DCIS.
Guiding Treatment and Improving Outcomes
After a cancer diagnosis, advanced breast imaging becomes even more critical for planning and monitoring treatment.
- Pre-operative staging: Breast MRI is the go-to tool for understanding the true extent of the disease. It accurately measures tumor size, detects multiple tumors, and checks the opposite breast, which is essential for planning the right surgery.
- Supporting breast conservation: For patients opting for a lumpectomy, MRI’s detailed mapping helps surgeons remove all cancerous tissue while preserving healthy breast. MRI findings alter surgical plans for about 25% of patients, ensuring a more custom approach.
- Assessing treatment response: When chemotherapy is given before surgery (neoadjuvant therapy), breast MRI is the most accurate method for monitoring if the tumor is shrinking. This allows for treatment adjustments and informs the surgical plan.
- Post-treatment surveillance: Advanced imaging remains important for follow-up, especially for patients with dense breasts or complex surgical changes.
By personalizing care, advanced imaging leads to better outcomes. Staying current with these practices is essential, and continuing education covers key topics to keep you at the forefront. You can explore 7 Topics You Will Cover in Mammography Continuing Education.
Conclusion
We’ve come a long way together on this journey through breast cancer detection. What started as a single X-ray view has blossomed into a sophisticated array of tools that help us see what we couldn’t see before. This shift toward advanced breast imaging isn’t just about better technology—it’s about better care for every patient who walks through your imaging suite door.
Think about where we started: traditional 2D mammography, a workhorse that has served us well but struggles with dense breast tissue. Then we explored Digital Breast Tomosynthesis, which slices through tissue overlap like flipping through the pages of a book. We finded how Breast MRI brings best sensitivity for our high-risk patients, catching cancers that might slip past other methods. Molecular Breast Imaging showed us how looking at cell activity rather than just structure can reveal hidden cancers in dense breasts. And we glimpsed tomorrow’s possibilities—Contrast-Improved Mammography, Ultrasound Elastography, and AI-assisted analysis—all working to make detection earlier, more accurate, and more comfortable for patients.
Here’s what matters most: early and accurate detection saves lives. These advanced techniques aren’t just impressive technology. They help you find cancers sooner, spare patients from unnecessary callbacks and biopsies, and guide surgeons toward more precise treatment plans. Every improvement in detection means someone’s mother, sister, or friend gets a better chance at beating this disease.
But here’s the thing—technology only works when the people using it understand it deeply. The field changes fast. What was cutting-edge five years ago is now standard practice. What’s experimental today might be routine tomorrow. That’s why your commitment to learning isn’t just about checking boxes for licensure. It’s about being the kind of professional who can confidently guide patients through their options and use these powerful tools to their fullest potential.
At Scrubs CE, we get it. You’re busy. You need education that fits your schedule and actually teaches you what you need to know. That’s why we’ve built courses that are self-paced, practical, and focused on real-world application. We want you to finish a course and think, “I can use this tomorrow.”
Ready to deepen your expertise in this dynamic field? Explore our comprehensive Mammography CEUs and find courses designed specifically for professionals who care about staying current. Your dedication to learning directly translates to better outcomes for your patients—and that’s what this is all about. Let’s keep learning together, because every image you interpret could be the one that changes someone’s life.

Recent Comments